Acute Coronary Syndrome (ACS) is a term used to describe a range of conditions associated with a sudden reduction of blood flow to the myocardial tissue. Three conditions come under the ACS category and they are Unstable Angina (UA), Non-ST elevation myocardial infarction (NSTEMI) and ST elevation myocardial infarction STEMI.
UNSTABLE ANGINA (UA)
Unstable angina is an acute coronary syndrome characterised by the absence of biochemical evidence of myocardial damage. Typical clinical features include prolonged retrosternal chest pain and other angina like symptoms that occur at rest. The 12 Lead ECG may show ST depression, localised T-wave depression or it may be normal (1).
NSTEMI - NON ST ELEVATION MYOCARDIAL INFARCTION
NSTEMI is an acute ischaemic event that causes necrosis of cardiomyocytes. Similarly to unstable angina, 12 Lead ECG may show ST depression, T-wave inversion or have no specific changes. The distinction between UA and NSTEMI is the presence of elevated cardiac biomarkers in blood samples (1).
STEMI - ST ELEVATION MYOCARDIAL INFARCTION
STEMI is characterised by myocardial necrosis secondary to prolonged ischaemia. It is confirmed by symptomology consistent with ACS and ST segment elevation in two or more anatomically contiguous leads on a 12 Lead ECG. In addition to increased levels of serum cardiac biomarkers (1).

This StudyGuide will focus on on the recognition and pre-hospital management of STEMI - ST Elevation Myocardial Infarction.
OVERVIEW
An acute myocardial infarction (AMI) is defined as myocardial necrosis secondary to prolonged myocardial ischeamia. An AMI occurs when blood flow to a particular region of myocardial tissue is significantly decreased, typically due to a rupture of an atherosclerotic plaque which causes a thrombotic occlusion of one or more coronary arteries. It is diagnosed based off clinical signs of ischaemia, elevated cardiac enzymes cardiac troponin T (cTnT) and troponin I (cTnI) in blood samples, 12 Lead ECG and cardiac wall motion abnormalities upon imaging.
In the pre-hospital setting where diagnostic tools are not as readily available, paramedics must make clinical and diagnostic decisions based of the patient’s history, clinical presentation and interpretation of their ECG. The end goal in the management of AMI is cardiac reperfusion within the shortest time frame possible. This generally requires a procedure known as primary percutaneous coronary intervention (pPCI) or coronary angioplasty, and in areas where this service is not available, thrombolysis. Delays in reperfusion lead to irreversible cardiac cell death, which may have significant impacts on the patients quality of life.
Acute coronary syndrome and STEMI’s are seen frequently by Australian paramedics, and it is one of the leading causes of death worldwide. Having a knowledge of the risk factors and most likely clinical presentation may help identify patients at risk of STEMI.
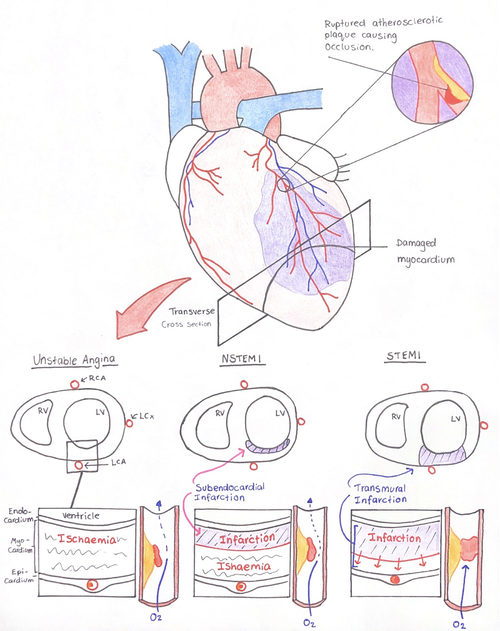
Figure 1: Transverse cross sectional image of the heart, shows the differentiating pathophysiology between variants of ACS.
RISK FACTORS OF AMI ACCORDING TO THE AUSTRALIAN HEART FOUNDATION
-
Male
-
Increasing age
-
Hypertension
-
Hyperlipidaemia
-
Obesity
-
Smoking
-
Diabetes mellitus
-
Family history
CLINICAL PRESENTATION OF AMI
Clinical signs and symptoms can vary person to person. Women and patients with diabetes in particular, may present with very atypical symptoms however still be having a coronary event.
-
Retrosternal chest pain - Often noted as a heaviness or crushing sensation. Also known to be a feeling of tightness or squeezing.
-
Pain that radiates up into the jaw, into the shoulders (primarily left side) and back.
-
Pale, diaphoretic and cool skin
-
Nausea and/or vomiting
-
Dyspnoea
RECOGNITION OF ACUTE MYOCARDIAL INFARCTION
The current method of AMI recognition in the pre-hospital setting is identification of clinical presentations consistent with acute coronary syndrome and 12 Lead ECG interpretation. AMI can be sub-categorised into ST elevation myocardial infarction (STEMI) and non-ST elevation myocardial infarction (NSTEMI). STEMI refers to an AMI with acute elevation of the ST segment on a 12 Lead ECG in two or more contiguous leads whereas there is no clear ST elevation in a NSTEMI. There may be other subtle changes on the 12 Lead including pathologic Q waves, T wave inversion or ST segment depression that suggest potential myocardial ischaemia, however there may not be any changes at all. For this reason, a 12 lead ECG alone is not an effective diagnostic tool in the setting of ACS.

Figure 2: 12 Lead ECG showing anatomically contiguous lead groupings (from our Emergency Clinical Cheats booklet you can find here).
12 LEAD ECG STEMI CRITERIA
-
Symptomology and history suggesting ACS.
-
New ST elevation at the J point of 1mm (0.1mV) or greater in 2 or more anatomically contiguous limb leads.
-
New ST elevation at the J point of 2mm (0.2mV) or greater in 2 or more anatomically contiguous precordial leads.
-
Reciprocal ST depression in contralateral leads confirms STEMI diagnosis.
-
No evidence of left bundle branch block (LBBB).
PRE-HOSPITAL MANAGEMENT OF STEMI

Figure 3:
Snapshot of a 12 Lead ECG with changes consistent with an Inferior STEMI. J point elevation of 3.5mm (0.35mV) from the isoelectric line in leads II, III and aVF. Reciprocal changes can be seen in I and aVL.
Paramedics are called out to chest pain many times everyday and thankfully most patients aren’t having a heart attack. However as previously mentioned, a 12 Lead ECG alone is insufficient as a diagnostic tool in the pre-hospital setting. The patient requires a blood test to identify cardiac damage. Any chest pain that sounds like it may be cardiac gets treated as such, until it can be ruled out at hospital. As the saying goes “treat for the worst, hope for the best”. STEMI on the other hand is a time critical emergency, as time is tissue. Recognition is a highly important factor in the patient receiving the correct care in a timely manner. For this reason paramedics receive constant refresher training to update and improve their ability to identify STEMI’s. Secondly, rapid transport to a cardiac capable hospital with the resources to reperfuse the ischaemic myocardium is also a priority.
ASSESSMENT AND TREATMENT GOALS
Reperfusion of the cardiac muscle is the primary goal when treating a STEMI, and that is done in the Cath Lab at a cardiac capable hospital. In the meantime, it is the paramedics responsibility to recognise the problem, begin the pharmacological treatment and deliver the patient to the lab. In order to achieve this, there are a few important actions and considerations.
-
We should conduct a timely assessment of the patient’s condition.
We should begin by taking a detailed history of the patients current complaint, including an OPQRST pain assessment, as well as the identification of other signs and symptoms. Vital sign assessment including the pallor and moisture of the patient’s skin. Assess risk factors that may increase the likelihood of AMI.
-
Obtain and examine a 12 Lead ECG.
Systematic assessment of the ECG to identify any potential ischaemia, infarction or other abnormalities. Examine for STEMI criteria. If positive, acknowledge time criticality and mobilise additional resources if required.
-
Consider differential diagnosis’ and STEMI mimics.
-
Initiate basic patient cares and pharmacological intervention.
Treatment of STEMI is multifactorial and requires a multitude of interventions. The focus is on the reduction of myocardial oxygen demand by reducing workload, inhibition of platelet aggregation with anti-platelet therapy, maintaining patient comfort through adequate pain relief and maintenance of normal vital signs with basic cares.
Pharmacological intervention indicated in STEMI treatment includes 300mg Aspirin. Sublingual GTN as primary pain relief provided there are nil contraindications. Fentanyl, the preferred opioid for additional pain relief in cardiac chest pain. Heparin and Ticagrelor for further anti-platelet therapy under the direction of the receiving interventional cardiologist. Anti-emetic and IV sodium chloride 0.9% is indicated for cardiogenic shock. Oxygen is indicated if the patient is hypoxic with Sp02 < 94% ra. More precise information can be obtained from state or service clinical guidelines.
-
Preparation of deterioration and rapid transport with pre-notification.
Defibrillation pads may be applied to the patient in preparation for a rapid resuscitation effort in the event of cardiac arrest.
Pre-notify the receiving hospital of your arrival if not already done, to allow a smooth transition through triage to the Cath Lab or resus bay.
Both STEMI and NSTEMI can be either life threatening or life altering emergencies. Rapid identification and solid knowledge of the physiology and treatment goals can go along way toward positive outcomes for our patients.
If you’ve made it this far, thank you!! If you want to hear about my first ever STEMI patient, click on this link to read about it!!

www.paramedicstudyguide.com.au

